A factual review of medical evidence that the cause of heart disease is NOT cholesterol and the use of statins has therefore been a failure. Reclaim your health by understanding the real factors driving disease.
Coronary heart disease (CHD) kills more than 370,000 people annually in the U.S.1 The standard of care for reducing this risk is to monitor a traditional lipid panel and fasting blood sugar despite clear evidence that these two tests are inefficient. It has been demonstrated that the majority of CHD occurs in patients with normal lipid panels. The 2013 ACC/AHA Guidelines on management of cholesterol and atherosclerotic disease ignored all evidence that more in depth testing such as LDL particle number, particle size, measurements of oxidized LDL, CRP or other easily obtainable markers hold any value despite ample evidence to the contrary.2-4
The use of fasting glucose as a measure of efficient glucose management by the body is still standard despite evidence that it fails to detect up to 40% of active type 2 diabetics or patients with active insulin resistance.5 Given that CHD is our number one killer in this country I want to propose an approach that goes beyond our current standard to expand into the integrative model of overall health. I have already discussed primary lab options in previous articles and want to direct discussion here to treatment options and approaches.6-7
The United States represents just 5% of the world population yet we consume 50% of all the drugs made globally. If drugs truly made us healthy then obviously we would have to be the healthiest people on the planet but clearly this is not the case. We rank 30th in life expectancy globally and hold the world record for rates of diabetes, cardiovascular disease and obesity. Following the 2013 ACC/AHA guidelines to offer statins to an ever widening audience and employing polypharmacy may help modify the disease progression but it doesn't allow us to truly reverse the course of the disease. To accomplish this we need to attack the cause. The modern integrative care physician or practitioner has an arsenal of tools available that have been shown to be far more effective at targeting the cause of the inflammation that drives CHD.
A brief exploration of the history of heart disease
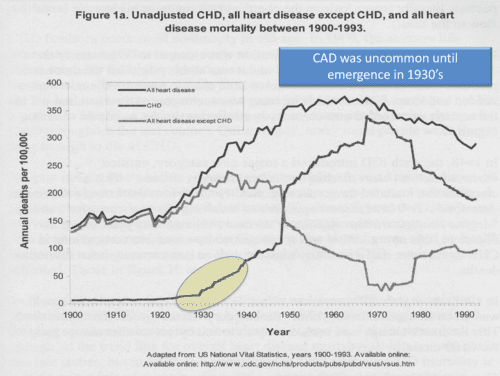
Exploring numbers from the CDC we can track the history of coronary heart disease to its origin in the 1930’s.8 The occurrence of heart disease from 1900 to 1930 was nearly all structural disease, valvular issues, aneurysms etc. Coronary heart disease (CHD) was rare. In 1930 we see the first stir of CHD as processed foods became more available to the American diet. Notice the dramatic skyrocket increase in CHD in 1950. What happened in 1950? The introduction of hydrogenated man-made oils to the American diet. Margarine was born and processed foods multiplied dramatically. We stopped eating food and began to eat man-made food-like substrates. This overlaps the advent of surgical techniques and Dr. DeBakey’s solutions for structural heart disease and soon we see death from structural heart disease plummet as CHD rises.
President Eisenhower’s myocardial infarction while in office in 1955, introduced America to a new vernacular.9-10 For the first time in history our nation was asking about the cause and condition of “heart attacks”. The AMA was overrun with demands by the public for an explanation and how to avoid this new disease. They had no answer and in frustration turned to Ancel Keys a nutritionist and scientist of the day that had loudly proclaimed the Lipid Hypothesis as an explanation for heart disease. His theories were incorrect but it gave birth to what lives today as the belief that fat causes heart disease.
Eisenhower took the advice of his physician and removed eggs and all forms of fat from the diet and increased his use of margarine and grains in the diet. His cholesterol continued to rise and he went on to have several more M.I.’s before he died in 1969. But as we look at Eisenhower’s disease history it is peppered with sources of inflammation including Crohns, arthritis and melanoma.10 It was his high carb inflammatory diet, his inflammatory bowel disease and stressful life that drove his ultimate demise.
Statin drugs were born in the late 1970’s and since then we have relied heavily on this growing group of drugs to corral what we thought was the cause of heart disease. By the 1990’s research had clearly shown that fat and cholesterol was not the cause of heart disease but getting that message conveyed to the public and to doctors is on ongoing challenge. Statins are efficacious agents in lowering the LDL but given that this is not the cause of heart disease the use of this approach as a sole methodology will lead to less than ideal results. The 2013 ACC/AHA guidelines, with 33% of its members working for statin manufacturers is not free of bias and they recommended the use of a “Risk Calculator” to be employed in determining who was in need of statin therapy. They admitted that they had no studies to show that use of this calculator was valid as it had not been tested in human trials.2 The Risk Calculator would dramatically increase the number of individuals that now qualify for statin use.
What is needed to return to CHD risk rates of the 1920’s is not more statin use but a return to healthy lifestyle and healthy diets. As Hippocrates once said, “Let food be thy medicine.” The 2013 ACC/AHA board failed to offer any meaningful guidance here. This board offered lip service to diet and lifestyle saying that these modalities should be used as “First Line” therapy but then fell short as they did not offer any guidance for the application of exercise and their only dietary insight was to employ the DASH diet. The DASH diet recommends the consumption of 6 to 8 pieces of bread daily. This recommendation needs to be questioned as the intake of a highly allergenic, high glycemic wheat products such as bread will most assuredly drive the very inflammatory process that in fact causes atherosclerotic disease.11-12
Before we leave the topic of statin drugs lets explore a few controversies that currently exist. Despite all of the grand statements made in defense of statins the truth is that we need to treat 1000 people in order to stop a mere 20 to 30 heart attacks. This benefit comes at a cost both financial and physical as statin use causes well-known side effects leading a full 40% of all statin users to stop therapy due to complications. If we were to compile all of the well known studies which include: JUPITER, CORONA, LIPID, WOSCOPS, PROSPER, MEGA, GISSI HF, GISSI PREV, ALLHAT, 4S, ASCOT-LLA, HPS, & AFCAPS/TEXCAPS we would have a total of 90,056 patients. One of the concerns expressed by many is that all of these studies are funded by the very pharmaceutical companies that produce the statin drugs being tested so there is inherent bias.
The largest statin study ever done was not funded by a statin manufacturer and needs to be included in our assessment if we are to arrive at an educated position. The Nilsson study was conducted in 2011 by a governmental agency seeking to assess the benefit of statins on reducing cardiovascular events and deaths.13 They studied 4 million people over 5 years and tracked use of statin therapy and reported that they saw no evidence that statins reduced cardiovascular events or risk. This study doesn't have a pharmaceutical funded bias and dwarfs the other studies in shear numbers.
The use of statins tripled over the 5-year period yet the number of myocardial infarctions and deaths from myocardial infarctions did not change significantly. In fact in subgroup analysis we saw that the occurrence rates of vascular events in men age 50-59 increased 19.5% despite a 310% increase in statin use. This warrants an explanation in light of our current fascination with statin therapy.
One explanation may be the rise in diabetic disease under the influence of statins. Statins cause diabetes and this has been shown in multiple studies.14-16 The Women’s Health Initiative, after stratifying for other risk factors, determined that the occurrence rate of diabetes directly due to the use of statins was 36 new diabetic cases out of 1000 people treated.14 Other studies such as PROSPER have confirmed this effect.17 We know that 80% of deaths in diabetic patients is due to vascular disease such as CHD and cerebral vascular accidents. Does the diabetic insult caused by statin use offset their benefit leaving us the results seen in the Nilsson study?
Studies show that CRP is twice as sensitive as LDL in predicating MI.18 CRP is more than just a marker of inflammation; CRP is an agent of harm as it reduces functionality of the insulin receptor itself. Lowering CRP is critical to reversing the vascular risk and its progression. Statins may offer a modest impact here but other tools such as hormonal balance, nutrition, neutraceuticals and lifestyle changes offer a greater impact and certainly with less adverse risk.19-22
Exploring the Cause
The field of epigenetics has been a remarkable teacher and changed the complexion of medicine. At least 90% of chronic disease is driven by environmental exposure and not the genome.23 If we are to keep pace with the science we need to embrace the idea that the quality of our food, our water and our environment dictate disease process. Inflammation comes at us from all directions including gut problems, poor sleep, stress, excess weight, hormones, dental and all sources of inflame that drive cytokine signaling. Food is the number one element to drive all of these issues. High glycemic, chemical laden food drives oxidation and food allergy. A body exposed to stress and poor sleep will spike cortisol and trend towards selection of higher glycemic foods and greater caloric intake. Stress of any kind drives weight gain and both will combine to create rolling inflammation.
Atherosclerosis begins as a disease of the subendothelium and the vessel wall in direct response to the foods and inflammatory milieu that we create.24 Long before the first plaque appears we can detect the inflammation lying below the endothelial surface and address it.
Cardiovascular disease is the result of uncontrolled inflammation.25 Inflammatory responses occur within the wall:
- Expression of adhesion molecules by endothelial cells
- Attachment of leukocytes to the arterial wall
- Vascular cell adhesion molecule-1 (VCAM-1) binds monocytes and T lymphocytes, preceding the appearance of macrophages
- Oxidized lipids and cytokines IL-1 and TNF-alpha induce VCAM-1 expression via nuclear factor-kB
- The presence of nitric oxide limits VCAM-1 but glucose and insulin presence retards nitric oxide production.
- Inflammation and oxidative stress drives production of monocyte chemoat- tractant protein-1 (MCP-1) recruiting monocytes and facilitating their penetration past the endothelium into the intima.
- Monocytes mature into macrophages and engulf lipoproteins and become foam cells.
- The atheroma is born and the atherosclerotic process is fed by daily habits.
Processed foods are by nature inflammatory foods due to their commonly low fiber content and added sugar. Processed grains may not taste sweet but their ability to breakdown quickly into simple sugars drives hyperglycemia, which in turn generates insulin rise. As insulin rises, triglycerides are stored and not used as cellular fuel leading to abundance and hypertriglyceridemia. The presence of sugar promotes yeast growth and oxidative stress in the gut and the lack of soluble fiber hinders maintenance of proper flora leading to gut disturbance. This collusion of events favors autoimmune vascular dysfunction and inflammation.26
The healthy antioxidant content of a whole foods diet blunts endothelial dysfunction. Phytonutrients such as carotenoids, flavonoids, and polyphenols from a vegetable based diet blocks vascular inflammation. Healthy fats such as omega 3 fatty acids and monounsaturated fats impact the caveolae of the endothelial cell wall to induce an anti-inflammatory signal.
The caveolae are invaginations in the wall of the endothelial cells and play a major role in cell signaling. Caveolin-1 is a natural protein found within the caveolae and influence cell signaling events, and can facilitate the development of atherosclerosis if stimulated by the inflammatory signaling network. Caveolin-1 is necessary to stimulate the intracellular TNF-α- induced NFкB-dependent induction of cyclooxygenase-2 and prostaglandin E2.27 Caveolin-1 is known to contribute to endothelial dysfunction thru its ability to reduce nitric oxide levels and increase ROS. Strategies to lower the level of caveolin-1 result in the opposite impact, an anti-inflammatory signal. If caveolin-1 is reduced we see reduced levels of proatherogenic VCAM-1. Here are some of the mechanisms shown to help down regulate caveolin-1:
- Reducing TNF-alpha and lipopolysaccharides (LPS) levels inhibits caevolin-1 activity
- Sulforaphane activates Nrf2 thus attenuating LPS induced endothelial activation.28
- Docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) displace caveolin-1 from caveolae in endothelial cells, causing increased (nitric oxide (N.O.) production and reduced ICAM-1 expression.29
- By contrast, omega 6 fatty acids increase caveolin-1 expression
- Green tea polyphenols, specifically EGCG, were able to reduce caveolin-1 levels.30
Caveolin-1 if provoked by inflammation promotes endothelial lipid accumulation in the subendothelial space and enhanced monocyte/ macrophage recruitment.
In 2002 Dr. Mark Houston pointed out the three distinct responses of the blood vessel as a result of inflammatory exposures:
- Oxidative stress – as a result of a reduced oxidative defense.
- Inflammatory response as outlined above.
- Autoimmune – involvement of CD4 T-helper cells and CD8 cytotoxic cells.
These three vascular responses that lead to atherosclerotic disease are commonly ignited by the simple choices we make in the customary course of daily events. To defuse this bomb we need to invest our collective energies in educating our patients about the impact of their choices. Integrative clinicians distinguish themselves by offering action not lip service to this important agenda.
Integrative Care & Solutions
“It is more important to know what type of person has a disease than what disease a person has.” said Hippocrates. If we are to change the mindset and thus the habits of our patients we need to understand them, their hurdles and then educate them appropriately. So lets venture into the terrain of the integrative physician. Lets explore the potential we all have to truly reverse cardiovascular disease and exceed the standard of care.
Lifestyle
A comprehensive lifestyle change has dramatic impact on all aspects of the inflammatory process. Exercise, optimal nutrition with fruits and vegetables, moderate alcohol consumption and smoking cessation reduces the risk of MI by 80%.31 The Lifestyle Heart Trial included a plant-based diet, exercise and stress management and showed a 5% regression of coronary plaque compared to the control group who demonstrated a 8% progression in plaque size in just 1 year.33
Gut Health & Food Allergies
The gut represents the heart and soul of the immune system as peyers patches line the intestines and respond to the millions of antigens that pass thru us each day. Therefore the gut microbiota are central in determining the pathogenesis of inflammatory induced obesity, CHD, atherosclerosis and type 2 diabetes.34 Gut microbiota play a key role in an individuals potential risk for autoimmune disease, cardiovascular inflammation and other chronic diseases.35 Microbial diversity and number is important in disease prevention and resiliency to maintain function. Lower diversity is observed in obesity, inflammatory bowel disease, meat-base dietary patterns, diabetes and CHD. Higher diversity in vegetarian based dietary patterns with high dietary fiber, non-digestible carbohydrates, resistant starches, SCFA prebiotics and probiotics have a lower incidence of diabetes and CHD.35
Nutrition
Studies consistently show that altering lifestyle and diet is more powerful than simple drug therapy. In the Becker trial at the Mayo Clinic, a Mediterranean style diet that removes high glycemic carbs in conjunction with exercise, basic omega 3 fatty acid supplementation, low dose red yeast rise and education outperformed simvastatin (40 mg) on all fronts.36 Significant elevation in valuable HDL was seen in the lifestyle group but not with statin use. Studies by Ornish and others have demonstrated reduction in plaque size with diet and lifestyle that was unobtainable through drug use.33
We have seen that oxidized-LDL is one of the best lab predictors for CHD. This simple test is inexpensive and greater than 400% more predictive than total LDL measures.37 Addressing the cause of oxidized LDL is key to reversing CHD. There are many toxins in our environment capable of unbalancing our redox potential but the greatest threat is the constant dietary threat from processed foods. It is estimated than Americans consume more than 150 pounds of sugar and that a full 20% of our caloric intake is from wheat. Today’s wheat contains a unique amylopectin A that is man made via hybridization.11 Its branching pattern and ease of breakdown creates a sharp rise in blood glucose and thus insulin that generates significant inflammation and oxidative stress.
The content of antioxidants in your diet has the ability to reduce CHD risk. In a study quantifying the antioxidant content of individual diets, those with the highest quality foods and antioxidant content had a 20% lower risk for cardiovascular disease.38
Glutamate is an amino acid commonly found in our food supply but in nature it is bound to protein and found in small amounts. When food manufacturers use a concentrated form known as monosodium glutamate (MSG) this is not natural or healthy and creates toxicity. Glutamate causes a loss in human cerebral endothelial barrier integrity through activation of NMDA receptor.39 Glutamate increases lipid peroxidation thus increases oxidized LDL. Through its interaction in the vascular beds and the endothelium it increases reactive oxygen species, reducing antioxidant protection such as superoxide dismutase and glutathione.40 This inflammatory food additive thus increases risk for CHD, alters neurologic balance between sympathetic and parasympathetic balance driving hypertension and atherosclerosis.
The greatest source of antioxidants in the diet is from plant-based foods such as vegetables. Each serving of fruit has roughly 100 more calories from sugar than vegetables and so even abuse of healthy fruit can be problematic. The soluble fiber in vegetables feed the gut flora, binds toxins, lowers both blood glucose and cholesterol levels and is critical for proper elimination.35 Plant based diets continue to demonstrate protection from heart disease in multiple studies and yet physicians continue to struggle with this simple recommendation and follow thru. How is it possible that we use our powers of persuasion to convince patients to undergo colonoscopies, painful injections, digital exams or all types of medical procedures yet we struggle mightily to persuade our patient to eat a health diet.
Asking a patient to give up inflammatory foods is paramount to success. Many physicians feel ill equipped for this discussion as food and nutrition was not taught in medical school and is not a part of our general operating procedure. There are many tools to aid success here. Work with a local dietitian, recommend reading material, offer classes and educational options in your office but most importantly hold your patient accountable for follow thru. The will succeed if you carefully monitor and insist.
Exercise
The benefits of exercise include the following41:
- Intense exercise can raise our anaerobic threshold, increase basal metabolic rate and reduce fat stores thus cytokine production.
- Strengthen your cardiovascular and respiratory systems, cardiac output and lowers resting heart rate.
- Stimulates osteoblast activity increasing bone density, preventing osteoporosis
- Exercise with intensity induces sweat, which reduces toxic burden from cells and can improve cell to cell signaling and endocrine function.
- Ease depression and help manage pain and stress
- Normalizes cortisol release through support of proper parasympathetic tone
- Prevent and manage diabetes through optimization of insulin receptor function
- Enhances better sleep patterns. Sleep loss is directly correlated with blood glucose and cortisol rise.
- Cognitive improvement: Exercise increases oxygen delivery to brain tissue allowing us to have greater mental stamina, more creativity of thought and promote greater problem solving ability.
- Exercise stimulates the production of an important brain protein called brain-derived neurotrophic factor that helps repair and function of neurons.
Naci reviewed 16 meta-analysis on the effectiveness of exercise on mortality outcomes across 4 conditions; secondary prevention of coronary heart disease, rehabilitation of stroke, treatment of heart failure, and the prevention of diabetes. In coronary heart disease the odds of mortality was reduced with use of statins, β blockers, angiotensin converting enzyme inhibitors and antiplatelets compared with control, whereas exercise interventions had a similar reduction but with wider confidence intervals.42 The authors stated; “When compared head to head in network meta-analyses, all interventions were not different beyond chance: there were no statistically detectable differences among any of the exercise and drug interventions in terms of their effects on mortality outcomes.” “When compared head to head in network meta-analyses, exercise interventions were more effective than anticoagulants and antiplatelets.” stated the authors. Our prescriptions need occur beyond the prescription pad to include proper physical training.
In a well publicized trial in the New England Journal from 2002, lifestyle including exercise was far superior to metformin in its ability to prevent pre-diabetics from advancing to diabetes.43 Lifestyle intervention reduced the incidence by 58% while metformin use only reduced it 31%.
Armed with this knowledge we have a responsibility to get our patients moving. There is a huge variety of exercise options and the knowledge base to implement different approaches can be daunting. Rely on experts to dispense this information but do not rely on random “Personalized Trainers”. Forge a relationship with trainers in your area and discuss your specific needs for your patient population. Develop a network of trusted options and track progress as your patients engage.
A simple text that I find very helpful for patients of all abilities is “The New Rules of Lifting Supercharged: Ten All-New Muscle-Building Programs for Men and Women” by Lou Schuler & Alwyn Cosgrove. Learn to rely on websites of your choosing that offer sound advice that is in alignment with your preferences. Search the website for tools that work in your practice.
Cortisol
Cortisol reflects one of the most destructive forces in our physiology when it is not kept in balance. The nature of modern life is wrought with over commitments on our time and resources leaving us exposed to high risk for HPA axis dysfunction and the unhealthy rise in cortisol. If we truly want to expose the cause of heart disease then it is critical to assess and modulate the action of cortisol. Many of us cheat our sleep, exercise and diet all in the name of “I don’t have time!”. The Caerphilly study looked at the simple ratio of cortisol to testosterone and how it related to CHD. The answer was clear to see that as cortisol rose higher, leading to suppression of testosterone, this shift in ratio easily predicted those at increasing risk for a vascular event, specifically CHD.44
Sustained elevation in cortisol will have the following negative impact:
- Blood glucose regulation leading to insulin resistance and diabetes
- Poor conversion of levothyroxine into its active liothyronine form.
- Drop in testosterone and dihydrotestosterone
- Reduced levels of adiponectin further driving insulin resistance
- Elevation in IL1, IL-6 and TNF-alpha, thus CRP
- Loss of muscle and bone mass
- Gut disturbance, dysbiosis and immune dysregulation
Meditation & Heart Rate Variability training reduces risk
Heart rate variability is a normal beat to beat variation that reflects the health and balance of the sympathetic:parasympathetic nervous system. Physiologic stress adversely impacts this leading to direct increased risk for hypertension and heart disease. The use of heart rate variability training (EM wave) has been shown to be extremely powerful in restoring balance. In a study comparing its use to drug therapy, the group using this relaxation technique experienced a significantly greater drop in systolic blood pressure compared to those on drug therapy.45
In a study employing meditation, subjects were asked to meditate daily for just 13 minutes and cortisol was tracked over a 3 month time frame. There was a consistent reduction in overall cortisol expression of 28% over time.46 This reduction in cortisol is critical to proper sleep and weight management, both factors for the reduction of CHD. Chronic stress leads to feeling of fatigue, drop in energy, increased irritability and hostility and these emotions have been linked to the development of insulin resistance.47
Hormones
The hormones estradiol and testosterone have dozens of roles to play in our normal physiology. Both impact blood sugar and cholesterol metabolism. Abnormally low levels of testosterone or estradiol will increase risk for diabetes, vascular inflammation and CHD.48-54 Restoring low testosterone to normal levels aids in the reversal of type 2 diabetes and metabolic syndrome. CHD occurrence in menopausal women drops 40-50% with the use of bio-identical estrogen.
Administration of testosterone to men with high CRP and low testosterone will in fact reduce CRP. There is a consistent inverse relationship between testosterone levels and CRP.55 Low testosterone states are predictive of diabetes and normalization of testosterone levels is therapeutic in the reversal of diabetes as it affects the mitochondrial restoration of ATP production.56-62
Sleep & Sleep Apnea
Sleep is key for recovery from daily oxidative stresses that are normal wear and tear. Poor sleep quality that lacks slow wave sleep or a short sleep cycle is directly linked to predictable rise in ghrelin, a drop in leptin and a rising BMI.63 The average nights sleep in American has shrunk from an average of 8 to 9 hours back in 1970 to an average of 6 hours as of 2004.
After just 2 nights of fragmented sleep, insulin sensitivity is reduced and craving patterns for high glycemic foods rise dramatically.64 General calorie intake rises and exercise is reduced following fragmented sleep. This combination will obviously lead to weight gain and all the elements of inflammatory chemistry are in place to drive CHD.65
Obstructive sleep apnea (OSA) is associated with considerable morbidity and mortality and is directly linked to CHD, hypertension and diabetes.66 OSA results in fatigue, loss of quality of life, weight gain and obesity. First line therapy includes CPAP but compliance is poor. The reality is that treatment of obesity and weight gain thru diet and lifestyle will greatly impact both risk for OSA and severity of OSA. Starting with a simple Epworth Score to identify those at risk is a great start. Be suspicious of any patient who reports snoring. Have a low threshold for ordering sleep studies and assessment for CPAP. If CPAP is unacceptable to the patient then refer them a local dentist familiar with the construction and use of dental appliances to help position the jaw and tongue in a more anterior position out of the airway. If unfamiliar with these approaches then contact The American Academy of Dental Sleep Medicine (AADSM) for a clinician in your area. Be very cautious to never use sedation in an effort to improve sleep if the patient has risk for apnea.
CONCLUSION
Coronary artery disease involves a complex web of factors and physiology but when we step back and assess the common pathways its easy to see that we have left the lifestyle of the 1920’s. We don't eat food anymore we consume food-like substrates that come from factories not fields. The things that do come from fields are often genetically manipulated and dangerous. Instead of talking on the back porch we text, tweet, email, Instagram and Facebook all day every day. Look around you – no one is looking back because everyone’s nose is buried in the screen in their hand.
We don't exercise our bodies, we don't walk and we don't stretch. We sit in soft seats and expand. We have lost our way. We are anxious and over committed and we surely don't sleep anymore.
The human condition needs a few simple things to thrive. Clean food and water. Good sleep. A little exercise or simple movement. A normal cortisol level reflective of a calm existence where stress is “managed” or at least balanced with meditation and exercise. Tolerating stress is not the same as effectively managing it and defusing it. If we are to claim victory as true “health” care providers then we must find a way to drive healthy lifestyle into our patients. We must become the leaders in educating our communities in healthy lifestyle choices. We have fabulous tools at our disposal as the internet is bursting with tools that are user friendly.
We need to offer options to our patients that can weave into the fabric of their current lives but more importantly help our patients see the damage they are creating if their life is destructive. To simply offer drug therapy as the totality of our solution is akin to fastening a seatbelt on our patients as they race at 100 MPH toward a brick wall. It may reduce the damage but its not going to stop the crash. We need instead to step inside the vehicle and apply the brake.
As physicians we have tremendous influence on what our patients think, believe, and do. We need to expand our powers of persuasion to include lifestyle.
REFERENCES
- http://www.cdc.gov/heartdisease/facts.htm
- Stone, Robinson, et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology, Nov 2013
- Johnston, Jernberg, et al. Improved Identification of Patients With Coronary Artery Disease by the Use of New Lipid and Lipoprotein Biomarkers. Am J Cardiol 2006;97:640–645
- Huang, Mai, et al. The oxidation ratio of LDL: A predictor for coronary artery disease. Disease Markers 24 (2008) 341–349
- Kraft, Joseph. Diabetes Epidemic & You, 2008
- Huber, Gary. Metabolic Syndrome and Cardiovascular Disease: A Look at the Mechanism that Drives This Inflammatory Process: Part 1 Understanding the Metabolic Problem. Townsend Letter, May 2013
- Huber, Gary. Metabolic Syndrome and Cardiovascular Disease: Testing and Treatment Part 2: Quantifying Risk and Review of Treatment Options. Townsend Letter, June 2013.
- http://www.cdc.gov/nchs/products/vsus.htm
- Gary Taubes, Good calories. Bad calories. 2007
- Eisenhowers health timeline - http://www.doctorzebra.com/prez/g34.htm
- Davis, William. Wheat Belly, 2011
- Perlmutter, David. Grain Brain, 2013
- Nilsson, Molstad, et al. No connection between the level of exposition to statins in the population and the incidence/ mortality of acute myocardial infarction: An ecological study based on Sweden’s municipalities. Journal of Negative Results in BioMedicine 2011, 10:6
- Culver, Ockene, et al. Statin Use and Risk of Diabetes Mellitus in Postmenopausal Women in the Women’s Health Initiative. Arch Intern Med. 2012;172(2):144-152.
- Nakata, Nagasaka, et al. Effects of statins on the adipocyte maturation and expression of glucose transporter 4 (SLC2A4): implicationsin glycaemic control. Diabetologia (2006) 49: 1881–1892
- Grover, Luthra, et al. Are statins really wonder drugs? Journal of the Formosan Medical Association (2013) 1-7
- Shepherd, Blauw, Murphy, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. The LancetVolume 360, Issue 9346, 23 November 2002, Pages 1623–1630
- Jain, Ridker. Anti-inflammatory effects of statins: clinical evidence and basic mechanisms. Nature Reviews – Drug Discovery Volume 4 Dec 2005
- Tchernof, Nolan. Weight Loss Reduces C-Reactive Protein Levels in Obese Postmenopausal Women 2002; 105: 564-569
- Heilbronn LK, Noakes M, Clifton PM. Energy restriction and weight loss on very-low-fat diets reduce C-reactive protein concentrations in obese, healthy women. Arterioscler Thromb Vasc Biol. 2001;21:968–970.
- Okita, Nishijima Can Exercise Training With Weight Loss Lower Serum C-Reactive Protein Levels? Arterioscler Thromb Vasc Biol. 2004; 24:1868-1873.
- Zhang, Gao, et al. Endogenous sex hormones and C-reactive protein in healthy chinese men. Clinical Endocrinology (2013) 78, 60–66
- Rappaport SM. Implications of the exposome for exposure science. Journal of Exposure Science and Environmental Epidemiology (2011) 21, 5–9
- Expert Review In Cardiovascular Disease 2010;8:821
- Libby, Peter. Inflammation and cardiovascular disease mechanisms.
- Mah, Bruno, et al. Postprandial hyperglycemia on vascular endothelial function: mechanisms and consequences. Nutr Res. 2012 Oct;32(10):727-40. doi: 10.1016/j.nutres.2012.08.002. Epub 2012 Sep 7.
- Wang, Lim, Toborek, Hennig. The role of fatty acids and caveolin-1 in tumor necrosis factor alpha-induced endothelial cell activation. Metabolism 2008;57:1328–39
- Zakkar, Van der Heiden, et al. Activation of Nrf2 in endothelial cells protects arteries from exhibiting a proinflammatory state. Arterioscler Thromb Vasc Biol 2009;29:1851–7.
- Li, Zhang, Wang, et al. Docosahexaenoic acid affects endothelial nitric oxide synthase in caveolae. Arch Biochem Biophys 2007;466: 250–9.
- Li, Ying, Zuo, et al. Green tea polyphenols down-regulate caveolin-1 expression via ERK1/2 and p38MAPK in endothelial cells. J Nutr Biochem 2009;20:1021–7.
- Yusuf, Hawken, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:937
- Ornish, Brown, et al. Lifetsyle Heart Trial. Lancet 1990; 336: 129-33.
- Piya, Harte, et al. Metabolic endotoxaemia: is it more than just a gut feeling? Curr Opin Lipidol. 2013 Feb;24(1):78-85.
- Gut microbiota and cardiometabolic outcomes: influence of dietary patterns and their associated components. Julia MW Wong Am J Clin Nutr 2014;100(suppl):369S–77S.
- Becker, Gordon, Morris, Yorko J, et al. Simvastatin vs therapeutic lifestyle changes and supplements: randomized primary prevention trial. Mayo Clin Proc. 2008 Jul;83(7):758-64.
- Johnston, Jernberg, et al. Improved identification of patients with coronary artery disease by the use of new lipid and lipoprotein biomarkers. Am J Cardiol. 2006 Mar 1;97(5):640-5.
- Rautiainen, Levitan, Orsini, et al. Total antioxidant capacity from diet and risk of myocardial infarction: a prospective cohort of women. Am J Med. 2012 Oct;125(10):974-80. doi: 10.1016/j.amjmed.2012.03.008.
- Sharp, Hines, et al. Glutamate causes a loss in human cerebral endothelial barrier integrity through activation of NMDA receptor. Am J Physiol Heart Circ Physiol 285: H2592–H2598, 2003.
- Li, Averill, et al. Differential roles for glutamate receptor subtypes within commissural NTS in cardiac-sympathetic reflex. Am J Physiol Regul Integr Comp Physiol. 2001 Sep;281(3):R935-43.
- Fragala, Kraemer, et al. Neuroendocrine-Immune Interactions and responses to exercise. Sports Med 2011; 41(8):621-639
- Naci, Loannidis. Comparative effectiveness of exercise and drug interventions on mortality outcomes: metaepidemiological study. BMJ 2013;347:f5577
- Knowler, Barrett-Connor, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002 February 7; 346(6): 393–403.
- Smith, Ben-Shlomo, et al. Cortisol, Testosterone, and Coronary Heart Disease : Prospective Evidence From the Caerphilly Study Circulation. 2005;112:332-340.
- Coherence: a novel nonpharmacological modality for lowering blood pressure in hypertensive patients. Glob Adv Health Med. 2012 May;1(2):56-64. doi: 10.7453/gahmj.2012.1.2.011.
- Vandana, Vaidyanathan, et al. Impact of integrated amrita meditation technique on adrenaline and cortisol levels in healthy volunteers. Evidence-Based Complementary and Alternative Med, Vol 2011 Article 1D
- Raikkonen, Keltikangas-Jarvinen, Adlercreutz, et al. Psychosocial stress and the insulin resistance syndrome. Metabolism 1996; 45:1533-8.
- Morgentaler, Miner, et al. Testosterone Therapy and Cardiovascular Risk: Advances and Controversies. Mayo Clin Proc. n February 2015;90(2):224-251
- Tibblin G, Adlerberth A, Lindstedt G, Bjorntorp P: The pituitary-gonadal axis and health in elderly men: a study of men born in 1913. Diabetes 45: 1605–1609, 1996
- Haffner SM, Shaten J, Stern MP, Smith GD, Kuller L: Low levels of sex hormone-binding globulin and testosterone predict the development of non-insulin-dependent diabetes mellitus in men. Am J Epidemiol 143: 889–897, 1996
- Stellato RK, Feldman HA, Hamdy O, Horton ES, McKinlay JB: Testosterone, sex hormone-binding globulin, and the development of type 2 diabetes in middle-aged men. Diabetes Care 23: 490–494, 2000
- Oh J-Y, Barrett-Connor E, Wedick NM, Wingard DL: Endogenous sex hormones and the development of type 2 diabetes in older men and women: the Rancho Bernardo Study. Diabetes Care 25: 55–60, 2002
- Svartberg J, Jenssen T, Sundsfjord J, Jorde R: The associations of endogenous testosterone and sex hormone-binding globulin with glycosylated hemoglobin levels, in community dwelling men: the Tromso Study. Diabetes Metab 30: 29–34, 2004
- Laaksonen DE, Niskanen L, Punnonen K, Nyysonen K, Tuomainen T-P, Valkonen V-P, Salonen R, Salonen JT: Testosterone and sex hormone-binding globulin predict the metabolic syndrome and diabetes in middle-aged men. Diabet es Care 27: 1036–1041, 2004
- Zhang, Gao†, et al. Endogenous sex hormones and C-reactive protein in healthy chinese men. Clinical Endocrinology (2013) 78, 60–66
- Pitteloud, Relationship betw T levels and insulin, Diabetes Care 2005 REF192 Smith, Insulin sensitivity, J.Clin.Endocrin.Metab. 2006
- Lowell, Shulman, Mitochondrial Dysfunction and Type 2 Diabetes, Science, January 21, 2005
- Mootha, PGC-1 -responsive genes involved in oxidative phosphorylation are coordinately down-regulated in human diabetes Nature Genetics 2003
- Philips, Pinkernell, et al. The association of hypotestosteronemia with coronary artery disease in men. Arterioscler Thromb. 1994;14:701-706
- Chou TM, Sudhir K, Hutchison SJ, Ko E, Amidon TM, Collins P, Chatterjee K. Testosterone induces dilation of canine coronary conductance and resistance arteries in vivo. Circulation. 1996;94: 2614 –2619.
- Hak AE, Witteman JC, de Jong FH, Geerlings MI, Hofman A, Pols HA. Low levels of endogenous androgens increase the risk of atherosclerosis in elderly men: the Rotterdam study. J Clin Endocrinol Metab. 2002;87: 3632–3639
- Muller M, van den Beld AW, Bots ML, Grobbee DE, Lamberts SW, van der Schouw YT. Endogenous sex hormones and progression of carotid atherosclerosis in elderly men. Circulation. 2004;109:2074–2079.
- Taheri, Lin, et al. Short Sleep Duration Is Associated with Reduced Leptin, Elevated Ghrelin, and Increased Body Mass Index. PLoS Medicine, December 2004, Volume 1, Issue 3
- Hursel, Rutters, et al. Effects of sleep fragmentation in healthy men on energy expenditure, substrate oxidation, physical activity, and exhaustion measured over 48 h in a respiratory chamber. Am J Clin Nutr 2011;94:804–8.
- Stamatakis KA, Punjabi NM. Effects of sleep fragmentation on glucose metabolism in normal subjects. Chest 2010;137:95–101.
- Trakada, Chrousos, et al. Sleep Apnea and its association with the Stress System, Inflammation, Insulin Resistance and Visceral Obesity. Sleep Med Clin. 2007 June ; 2(2): 251–261. doi:10.1016/j.jsmc.2007.04.003.





